Etavopivat reduced the rate of vaso-occlusive crises, increased hemoglobin levels, and improved hemolysis markers and fatigue in patients with sickle cell disease (SCD). The researchers presented 52-week data from the HIBISCUS trial at the ASH Annual Meeting.
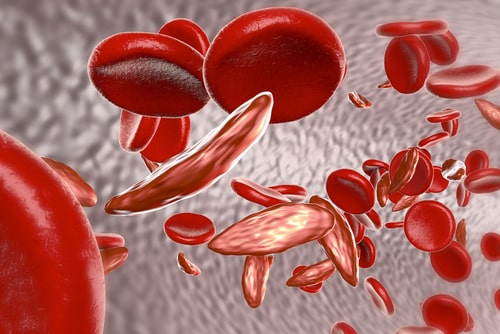
“Etavopivat is a potent, selective, once-daily, orally bioavailable activator of the red blood cell (RBC) pyruvate kinase isozyme, decreasing 2,3 DPG levels and increasing ATP levels in RBCs. In a phase 1 study, treatment with etavopivat in patients with SCD resulted in a rapid and sustained increase of hemoglobin (Hb) levels and decreased markers of hemolysis over 12 weeks,” explained the authors, led by Sophia Delicou of Hippokrateio General Hospital in Athens, Greece.
The HIBISCUS trial is a multicenter, phase 2/3, randomized, double-blind, placebo-controlled trial investigating the drug’s efficacy and safety in SCD. It enrolled 60 patients with any SCD genotype who were randomized to receive etavopivat 200 mg (n=21), etavopivat 400 mg (n=20), or placebo (n=19) once daily for 52 weeks. The researchers reported primary efficacy in the intent-to-treat (ITT) and per-protocol (PP) populations.
In the ITT population, at 52 weeks, vaso-occlusive crisis rates were 1.07 in the etavopivat 200 mg group, 1.06 in the 400 mg group, and 1.97 in the placebo group. The median time to a vaso-occlusive crisis was 33.6 weeks in both etavopivat groups and 16.9 weeks in the placebo group. At 24 weeks, Hb response was 38% in the etavopivat 200 mg group, 25% in the etavopivat 400 mg group, and 11% in the placebo group. The responses in patients receiving etavopivat occurred as early as week 2 and continued over 52 weeks.
In the PP population, at 52 weeks, VOC rates were 0.66 in the 200 mg group, 0.7 in the 400 mg group, and 1.77 in the placebo group. At week 24, Hb response was 46% in the 200 mg group, 33% in the 400 mg group, and 13% in the placebo group. In addition, all hemolysis biomarkers decreased from baseline in both etavopivat groups.
The study found that patients receiving etavopivat experienced improved fatigue. The drug was also well tolerated. Adverse events occurred in five patients in the etavopivat 200 mg group, four in the 400 mg group, and three in the placebo group. They included insomnia, hepatic enzyme increase, and Hb decrease. Adverse events were mild to moderate and resolved without intervention. Six participants in each etavopivat group and three in the placebo group discontinued treatment early.
“Based on the totality of data, proof of concept was established for etavopivat in SCD,” the researchers concluded.
https://ash.confex.com/ash/2024/webprogram/Paper204962.html
Reference
Delicou S, El Rassi F, Andemariam B, et al. Etavopivat reduces incidence of vaso-occlusive crises in patients with sickle cell disease: HIBISCUS trial phase 2 results through 52 weeks. Abstract #179. Presented at the 66th American Society of Hematology Annual Meeting and Exposition; December 7–10, 2024; San Diego, California.